Short Communication 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Implant Dentistry at a Prominent Crossroad!
*Corresponding author: Touradj Ameli, Diplomate, American Board of Prosthodontics, Diplomate, American Board of Oral Implantology/Implant Dentistry, Director, Boston Institute for Advanced Dental Education, Former, Faculty Instructor; Department of Restorative Dentistry and Biomaterials Sciences at Harvard University School of Dental Medicine, Former, Clinical Associate Professor; Department of Prosthodontics at New York University College of Dentistry, Practice Limited to Implant, Aesthetic and Reconstructive Dentistry,180 linden St, 8C, Wellesley, MA. USA.
Received: August 15, 2022; Published: September 02, 2022
DOI: 10.34297/AJBSR.2022.17.002308
Abstract
Keywords: Aging population, Dental implant, FP3, Fixed-prosthesis-3, Poly (methyl methacrylate), PMMA, Candida albican, Oral Squamous Cell Carcinoma (OSCC), Oral cancer
Introduction
The public and healthcare providers should know about the dark side of dental Implants before receiving them or even offering them as an ideal treatment option for replacing missing teeth. While dental implants are an excellent option for healthy patients, meticulous home care and routine two to three months, professional hygiene visits are critical. Dental implants are as much and even more susceptible to inflammation as natural dentition. Once the bacteria provoke the peri-implant tissue, a chronic inflammatory cascade could initiate undesirable consequences, including cancer.
Short Communication
The proliferating aging population in the United States has experienced improved health care, oral health-related quality of life, and longer life spans than the previous generations. With rising life expectancy, desire for dental care has become a more systematic effort to retain natural dentitions. However, due to the high cost of routine quality dental care and fixed income, along with other misleading information from social media, these populations find themselves at prominent crossroads; to save teeth or replace them with dental implants and related prostheses! Endosseous dental implants represent a great alternative to missing teeth but can also present an additional and measurable health problem, as the rate of this treatment modality is increasing rapidly. Initially, this novel idea was to restore the function of a severely resorbed jaw when wearing a mandibular conventional removable denture prosthesis was difficult and often painful. While many advancements have been made in implant dentistry, a few additional essential points must be considered to prevent serious health issues.
NIDCR Oral Health in America reports [1] that about 70% of older Americans already live with at least one or two form of a chronic disease. As these diseases progress, physical and neurobiological changes become more debilitating, effecting individual’s capacity to maintain good oral hygiene, hence, becoming more susceptible to serious oral health issues with the end point of tooth loss. Literature suggests that retention rates for natural teeth are on the rise, creating optimism for a significant reduction in the demand for Poly Acrylic (methyl methacrylate) [PMMA] based removable prostheses [2,3]. However, the current trends in dentistry refute this idea as more adult patients experiencing partial or complete state of edentulism by being encouraged to remove teeth in favour of replacing with dental implants and related prosthesis. The negative impact of this shift must be recognized before we encounter a new pandemic related to the adverse effect of implant dentistry on quality of life and overall hike in healthcare cost. This short article reminds us how microbiome alteration from dental implant treatment has the potential to severely affects an individual’s host response.
The most critical factor in implant dentistry is patient selection; a dental implant is a prosthetic device surgically inserted into one of the most challenging areas within the human body. The human oral cavity is home to a complex and diverse microbial ecosystem, harboring over 700 species of bacteria, often with protective role against the invasion of undesirable outside provocation. It also nurtures numerous other microorganisms, which include fungi, viruses, and protozoa [4]. The surfaces of hard tissue and soft tissue of the oral cavity include the gingival sulcus, the tongue, the cheek, the hard and soft palates, the floor of the mouth, the throat, the saliva, and the teeth, serve as a natural environment and suitable niche for the colonization of the microbes which have complementary receptors for adhesion. With the alteration of the ecosystem, the shifts in microbiome composition are inevitable, as the imbalance of symbiotic relationship between the microorganisms allows the pathogenic species to breach the barrier of the commensals and adhere to the host tissue. The imbalance of microbial flora contributes to oral and systemic dysbiosis, leading to a range of undesirable ill conditions and cancer [5].
The association between microbiota and cancer has been known since the early 19th century. While the classic contributing pathway in promoting cancer through genetic mechanisms, epithelial injury, or chronic inflammation was proposed by Virchow 150 years ago [6], recent evidence suggests that human disease is attributable not only to single pathogens but also to dynamic changes in our microbiome [7,8]. The human microbiota is highly personalized and systematically varied. The salivary microbiota community is highly fluctuating compared to the rest of the body, and the composition and formation are associated with the general health or lack thereof [9-11]. The oral microbiome consists of a core microbiome and a variable microbiome. The core microbiome exists under healthy conditions; the variable microbiomes are exclusive to any individual, in a constant state of flux, and fluctuate with nutrition, age, geography, use of medications, including antibiotics/probiotics, genetic determinants, and other environmental influences such as smoking and even selection of dental materials [12].
The most commonly affordable and cost-effective material used for fabricating Implant -prosthesis involves polymethylmethacrylate (PMMA) The absence of ionic charge on PMMA surface properties creates an imbalance environment for selective adsorption of cationic peptides salivary antimicrobials such as defensins and histatins, not only minimizes the adsorption of defence molecules, but the attractive London-van der Waals forces facilitates the adherence of C. albicans on the denture surface, leading to denture stomatitis [13-16].
Upon adhesion to a surface (biomedical material or tissue), replication adherent bacteria can secrete mostly insoluble gelatinous biopolymers, forming a matrix known as a biofilm. All commensal and pathogenic microorganisms form biofilmlike alliances that attach themselves to the tissue, including teeth or biomaterial surfaces. Consequently, they have profound implications for the host as microorganisms growing as biofilms are significantly less susceptible to antibiotics and host defences than are planktonic forms of the same microorganisms. Many biofilm infections are complicated to resolve and commonly manifest as chronic or recurrent infections. Biofilm infections constitute many clinical challenges, including diseases involving uncultivable species, chronic inflammation, impaired wound healing, rapidly acquired antibiotic resistance and the spread of infectious emboli [17].
Regardless of the sophistication of the biomedical Implant, all medical devices or tissue engineering biomaterials constructs are susceptible to microbial colonization and infection [18]. The formation of biofilms on implants and biomaterials in medicine and dentistry has been known to cause significant morbidity [19,20]. In particular, the adhesion of Candida albicans on polymethylmethacrylate (PMMA) materials has been recognized as a problem for decades; that along with poor hygiene is thought to be the culprit in the development of Candida-associated denture stomatitis [21-23].
Mounting evidence has supported a correlation between Candida infection and the development of oral epithelial dysplasia [24]. Furthermore, researchers claim candidiasis might not just be randomly coexisting with oral cancer, but possibly C. Albicans may initiate or facilitate the development of dysplastic lesions or Oral Squamous Cell Carcinoma (OSCC), the most common malignant epithelial neoplasm of oral cavity [25].
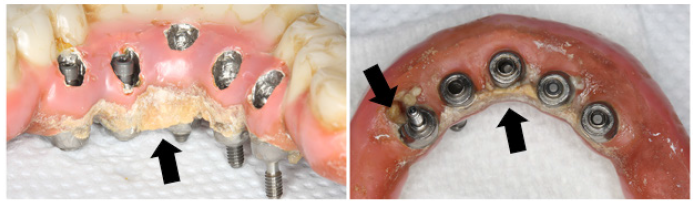
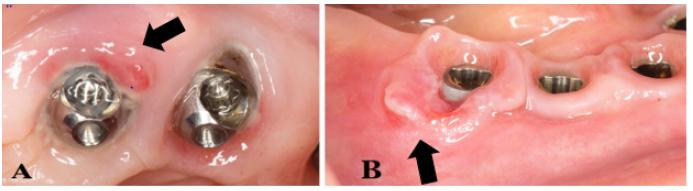
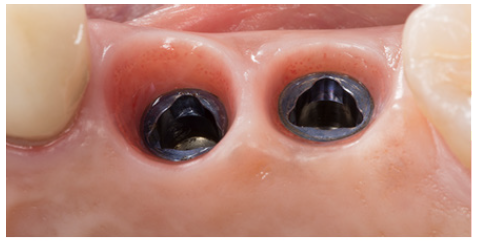
Osseo integrated implants are a safe and efficient treatment modality for dental and oral rehabilitation. One of the most common complications of endosseous implants is peri-implant inflammation, which is associated with the disturbance of the normal microbiome, affecting the soft and hard tissues surrounding the implants [26]. It clinically appears as an erythematous lesion with edema, occasionally ulcerated, sometimes painful, with bleeding and presence of an inflammatory exudate. OSCC with the erythroplakia appearance could be easily mistaken with peri-implantitis disease as it can mimic a benign inflammatory condition. A biopsy is highly recommended when conventional treatment fails to resolve the lesion or in some cases if its appearance is sudden and severe [27]. Although common sites for OSCC to develop are on the tongue, lips and floor of the mouth and around inflamed peri-implant area [28,29], the author has also seen a clinical case associated with mucosa around dental implants of a 68 years of age female restored with fixed implant Metal-acrylic resin (PMMA) prostheses FP3 [30], on both maxillary and mandibular arches (Figure 1 & 2), referred to practice for urgent consultation due to pain and discomfort of soft tissue around mandibular implants (Figure 3), upon suspicion patient was referred back to the treating dentist, in her hometown, and later pathology report confirmed OSCC diagnose (Figure 1-4).
Conclusion
Peri-implantitis is a risk factor for developing OSCC when it remains unresolvable. Implants’ long-term success and survival depend on the healthy soft tissue around implants (Figure 4); selecting the right patient, proper materials, treatment design, and post-treatment routine maintenance are crucial, as biofilm development and altering normal microbiota are inevitable.
Conflict of Interest
No conflict of interest.
Acknowledgement
Tannaz Shapurian, DMD, MSc, Diplomate, American Board of Periodontology, Associate Professor; Department of Periodontology, Tufts University, School of Dental Medicine.
References
- (2022) NIHDCR; Oral Health in America, 2022 Bulletin; Section 3B Summary.
- Marcus PA, Joshi A, Jones JA, Morgano SM (1996) Complete edentulism and denture use for elders in New England. J Prosthet Dent 76(3): 260-266.
- Marcus SE, Drury TF, Brown LJ, Zion GR (1996) Tooth retention and tooth loss in the permanent dentition of adults: United States, 1988-1991. J Dent Res 75(Spec No): 684-695.
- Dewhirst FE, Chen T, Izard J, Paster BJ, Tanner AC, et al. (2010) The human oral microbiome. J Bacteriol 192(19): 5002-5017.
- Avila M, Ojcius DM, Yilmaz O (2009) The oral microbiota: Living with a permanent guest. DNA Cell Biol 28(8): 405-411.
- Virchow R (1863) Die krankhaften Geschwülste: Virchow R, editor. Verlag von August von Hirschwald pp. 57-101.
- Turnbaugh PJ, Ruth E Ley, Michael A Mahowald, Vincent Magrini, Elaine R Mardis, et al. (2006) An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 444(7122): 1027-1031.
- D Alessandro G, Antonangeli F, Marrocco F, Porzia A, Lauro C, et al. (2020) Gut microbiota alterations affect glioma growth and innate immune cells involved in tumor immunosurveillance in mice. Eur J Immunol 50(5): 705-711.
- Costello EK, Relman DA (2014) Population health: immaturity in the gut microbial community. Nature 510(7505): 344-345.
- Anukam KC, Agbakoba NR (2017) A comparative study of the oral microbiome compositions of healthy postmenopausal, premenopausal, and prepubertal Nigerian females, using 16s rrna metagenomics methods. Niger J Clin Pract 20(10): 1250-1258.
- Ogawa T, Hirose Y, Honda OM, Sugimoto M, Sasaki S, et al. (2018) Composition of salivary microbiota in elderly subjects. Sci Rep 8(1): 414.
- Zarco MF, Vess TJ, Ginsburg GS (2012) The oral microbiome in health and disease and the potential impact on personalized dental medicine. Oral Dis 18(2): 109‐120.
- Edgerton M, Levine MJ (1992) Characterization of acquired denture pellicle from healthy and stomatitis patients. J Prosthet Dent 68(4): 683-691.
- Klotz S, Drutz D, Zajic J (1985) Factors governing adherence of Candida species to plastic surfaces. Infect Immun 50(1): 97-101.
- Klotz S (1994) The contribution of electrostatic forces to the process of adherence of Candida albicans yeast cells to substrates. FEMS Microbiol Lett 120(3): 257-262.
- Li J, Hirota K, Goto T, Yumoto H, Miyake Y, et al. (2012) Biofilm formation of Candida albicans on implant overdenture materials and its removal. J Dent 40(8): 686-692.
- James D Bryers (2008) Biotechnol Bioeng 100(1): 1-18.
- Bryers JD, Ratner BD (2004) Bioinspired implant materials befuddle bacteria. ASM News 70(5): 232-237.
- Kojic EM, Darouiche RO (2004) Candida infections of medical devices. Clin Microbiol Rev 17(2): 255-267.
- Khatoon Z, McTiernan CD, Suuronen EJ, Mah TF, Alarcon EI, et al. (2018) Bacterial biofilm formation on implantable devices and approaches to its treatment and prevention. Heliyon 4(12): e01067.
- Budtz Jörgensen E (1978) Clinical aspects of Candida infection in denture wearers. J Am Dent Assoc 96(3): 474-479.
- Ramage G, Tomsett K, Wickes BL, López Ribot JL, Redding SW, et al. (2004) Denture stomatitis: A role for Candida biofilms. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 98(1): 53-59.
- Kulak Ozkan Y, Kazazoglu E, Arikan A (2002) Oral hygiene habits, denture cleanliness, presence of yeasts and stomatitis in elderly people. J Oral Rehabil 29(3): 300-304.
- Mc Cullough M, Jaber M, Barrett AW, Bain L, Speight PM, et al. (2002) Oral yeast carriage correlates with presence of oral epithelial dysplasia. Oral Oncol 38(4): 391-393.
- Vadovics M, Ho J, Igaz N, Alföldi R, Rakk D, et al. (2022) Candida albicans Enhances the Progression of Oral Squamous Cell Carcinoma In Vitro and In Vivo. mBio 13(1): e0314421.
- Kröger A, Hülsmann C, Fickl S, Spinell T, Hüttig F, et al. (2018) The Severity of Human Peri-Implantitis Lesions Correlates With the Level of Submucosal Microbial Dysbiosis. J Clin Periodontol 45(12): 1498-1509.
- Y Nariai, T Kanno, J Sekine (2016) Histopathological features of secondary squamous cell carcinoma around a dental implant in the mandible after chemoradiotherapy: a case report with a clinicopathological review. J Oral Maxillofac Surg 74(5): 982-990.
- Seo MH, Myoung H, Lee JH, Kim SM, Lee SK, et al. (2019) Changes in oncogenic protein levels in peri-implant oral malignancy: a case report. Maxillofac Plast Reconstr Surg 41(1): 46.
- Block MS, Scheufler E (2001) Squamous cell carcinoma appearing as peri-implant bone loss: a case report. J Oral Maxillofac Surg 59(11): 1349-1352.
- Misch CE (2014) Dental Implant Prosthetics. (2nd) Netherlands: Elsevier Health Sciences.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.